Tuberculosis is a contagious and potentially deadly disease. Its diagnosis can be challenging but specific characteristics on lung ultrasound can raise suspicions and trigger further investigations to pick up this disease earlier in patients.

SHARE
TABLE OF CONTENTS
Tuberculosis (TB) is a potentially serious infectious disease caused by the bacterium Mycobacterium tuberculosis. It primarily affects the lungs but can also affect other parts of the body, such as the brain, spine, or kidneys. TB is spread through the air when an infected person coughs or sneezes, releasing tiny droplets containing the bacteria, which can then be inhaled by others.
The symptoms of TB can vary depending on the stage of infection and the part of the body affected but commonly include a persistent cough, chest pain, coughing up blood, fever, night sweats, and weight loss. TB can be latent, meaning the bacteria are in the body but not causing symptoms, or active, where symptoms are present, and the person is contagious.
There are several diagnostic methods used to detect tuberculosis (TB) in patients. These methods vary in their sensitivity, specificity, and availability in different healthcare settings. Below are some common diagnostic methods:
This test involves injecting a small amount of purified protein derivative (PPD) tuberculin into the skin of the forearm. After 48 to 72 hours, a healthcare provider checks for a reaction at the injection site. A positive reaction indicates exposure to the TB bacteria, but it doesn't necessarily mean active disease. Further testing is usually needed to confirm active TB.

IGRAs are blood tests that measure the release of interferon-gamma by T cells in response to TB-specific antigens. These tests are used as alternatives to the TST, particularly in populations where BCG vaccination may interfere with TST interpretation.
This method involves examining sputum samples under a microscope to detect the presence and growth of Mycobacterium tuberculosis. While microscopy is rapid, it has limited sensitivity, especially in patients with a low bacterial load. On the other hand, culture is highly specify but is slower than microscopy, typically taking several weeks for results.
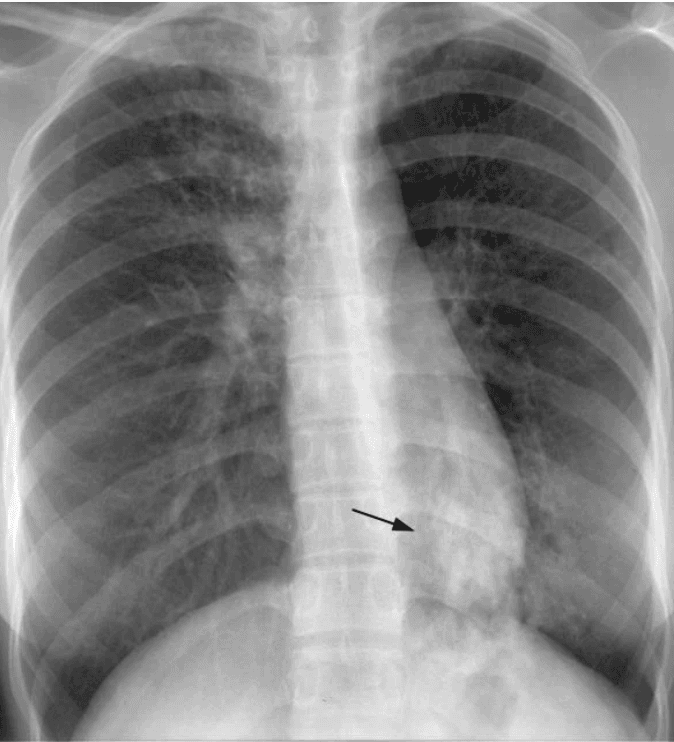
Chest X-rays can reveal abnormalities in the lungs suggestive of TB, such as cavities, consolidations, or infiltrates. While not specific for TB, chest X-rays are often used as an initial screening tool and to monitor disease progression or response to treatment.
Lung ultrasound can be a valuable tool in the diagnosis and management of TB patients, particularly in settings where other imaging modalities such as chest X-ray or computed tomography (CT) scan may not be readily available or feasible. While lung ultrasound findings in TB can vary depending on the stage and extent of the disease, some distinct features may be picked up.
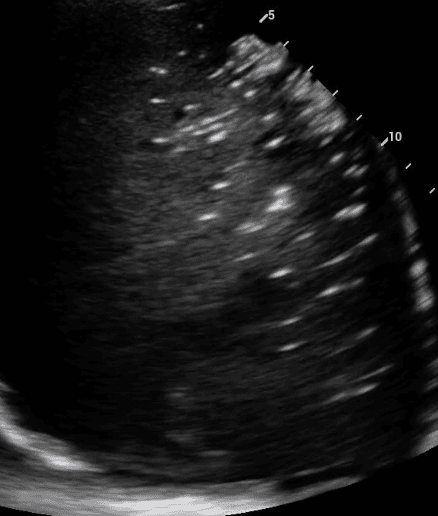
Subpleural nodules are small rounded areas of abnormal tissue growth that occur beneath the pleura, which is the thin membrane that covers the surface of the lungs. Granulomas are small, localized areas of inflammation that occur in response to infections, foreign substances, or immune reactions. They are especially common in tuberculosis.
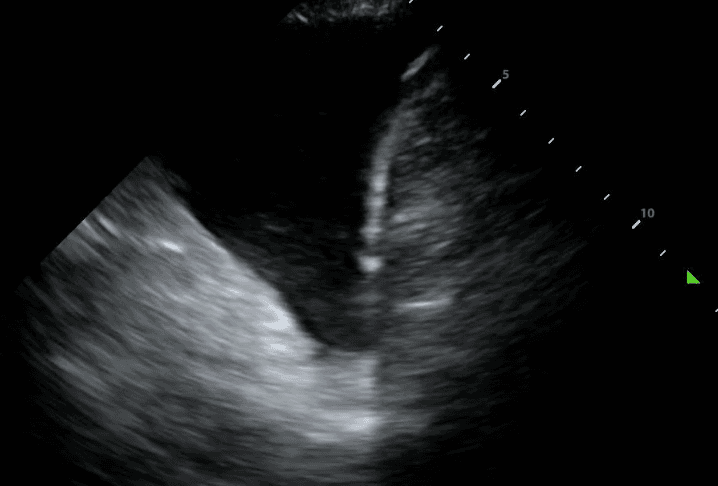
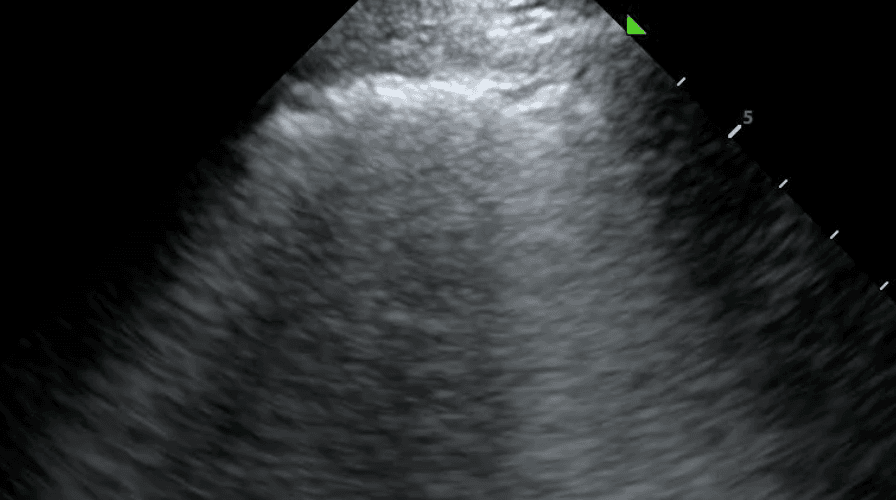
TB can lead to the accumulation of fluid in the pleural space, resulting in a pleural effusion. The incidence of these effusions range from 3% to 30% depending on the prevalence of TB and comorbidities such as HIV. On lung ultrasound, pleural effusion typically appears as anechoic (black) or hypoechoic (dark) fluid collection between the lung and the chest wall. The presence of pleural effusion in TB may indicate complications such as pleural TB or concurrent bacterial infection.
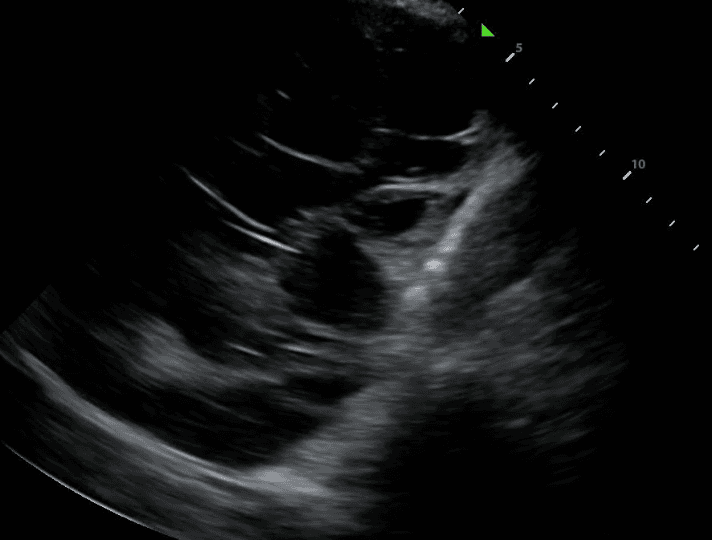
Lung ultrasound will also demonstrate diseased lungs that are filled with fluid or cellular debris. Lung consolidations often have bright air bronchograms, which represent air trapped in fluid filled bronchi.
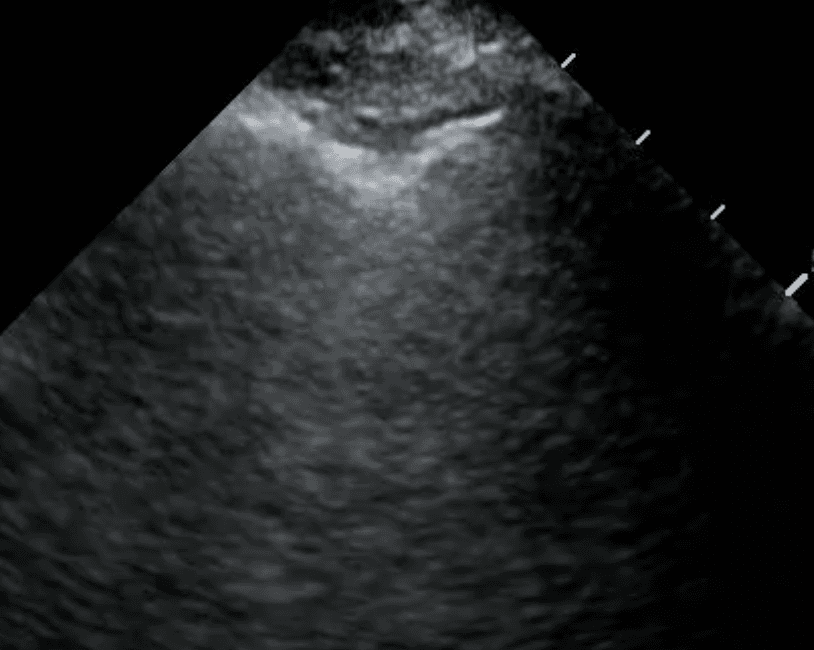
Chronic TB infection can lead to thickening of the pleura, the membrane lining the inside of the chest cavity and covering the lungs. Pleural thickening may be visualized as hyperechoic (bright) bands or irregularities along the pleural line on lung ultrasound (read more here). This finding is often associated with fibrotic changes and can be indicative of prior or active TB infection.
TB commonly affects the lymph nodes in the chest, leading to enlargement (lymphadenopathy). Enlarged lymph nodes may be visualized as dark or heterogeneous masses adjacent to the bronchi or blood vessels on lung ultrasound. In TB patients, mediastinal or hilar lymphadenopathy may be observed, indicating regional lymph node involvement.
In conclusion, POCUS offers several clues to the diagnosis of TB and has the advantage of being real-time, radiation-free, and cost-effective. Its ability to promptly detect TB-related abnormalities in diverse clinical settings, makes it an indispensable tool for frontline healthcare providers involved in TB diagnosis and management.
References
Catanzano, T. M. (2022, July 8). Primary tuberculosis imaging. Practice Essentials, Radiography, Computed Tomography. https://emedicine.medscape.com/article/358610-overview?form=fpf
Centers for Disease Control and Prevention. (2016, March 20). Basic TB facts. Centers for Disease Control and Prevention. https://www.cdc.gov/tb/topic/basics/default.htm
Kraft, C., Lasure, B., Sharon, M., Patel, P., & Minardi, J. (2018). Pediatric lung abscess: immediate diagnosis by point-of-care ultrasound. Pediatric Emergency Care, 34(6), 447-449. https://journals.lww.com/pec-online/abstract/2018/06000/pediatric_lung_abscess__immediate_diagnosis_by.18.aspx
Mayo Foundation for Medical Education and Research. (n.d.). Tuberculosis. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/tuberculosis/diagnosis-treatment/drc-20351256
Mongodi, S., Bonaiti, S., & Mojoli, F. (2023). Ultrasound assessment of pulmonary abscess. Medicina intensiva, 47(5), 304. https://www.sciencedirect.com/science/article/pii/S2173572722002399?via%3Dihub
Prina, E., Torres, A., & Carvalho, C. R. (2014). Lung ultrasound in the evaluation of pleural effusion. Jornal brasileiro de pneumologia : publicacao oficial da Sociedade Brasileira de Pneumologia e Tisilogia, 40(1), 1–5. https://www.scielo.br/j/jbpneu/a/vKCk7TwXRn34RwMyTHRgK3c/?lang=en
Saoud, M., Patil, M., Dhillon, S. S., Alraiyes, A. H., Sunar, U., & Harris, K. (2017). Image characteristics of lung abscess by convex-probe endobronchial ultrasound. Journal of Bronchology & Interventional Pulmonology, 24(3), 34-35. https://journals.lww.com/bronchology/citation/2017/07000/image_characteristics_of_lung_abscess_by.20.aspx
WebMD. (n.d.). TB tests: Types of tuberculosis tests and results. WebMD. https://www.webmd.com/lung/tests-tuberculosis
SHARE
© 2025, DEEP BREATHE, INC