Lung ultrasound is superior to chest x-ray in differentiating between pneumonia and atelectasis. This distinction is important when caring for sick patients. Read on to learn how to use lung ultrasound to distinguish between these two diseases.

SHARE
TABLE OF CONTENTS
A recent meta-analysis and systematic review highlighted lung ultrasound's superior sensitivity compared to chest x-ray in detecting lung consolidations among sick patients (read more about lung consolidations here). Determining whether these consolidations represent pneumonia is important to properly care for patients. This post will aim to provide you with the tools to systematically differentiate atelectasis and pneumonia using lung ultrasound.
Ultrasound is superior to chest-xray in differentiating between atelectasis and pneumonia, with a sensitivity of 91.67% and specificity of 100%. The two key features of pneumonia on lung ultrasound are dynamic air bronchograms and increased blood flow within a lung consolidation.
Dynamic air bronchograms visualize air movement within consolidated lung regions and are highly specific for pneumonia. This finding effectively rules out atelectasis, which only has static air bronchograms.
Assessing blood flow in lung tissue is another valuable tool, with 90% sensitivity and 68% specificity in detecting pneumonia. When consolidation shows high blood flow, pneumonia tends to be the underlying diagnosis. The next section will add further qualitative measures to use in your assessment of a lung consolidation.
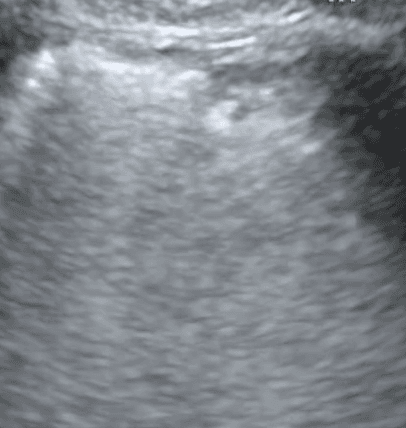
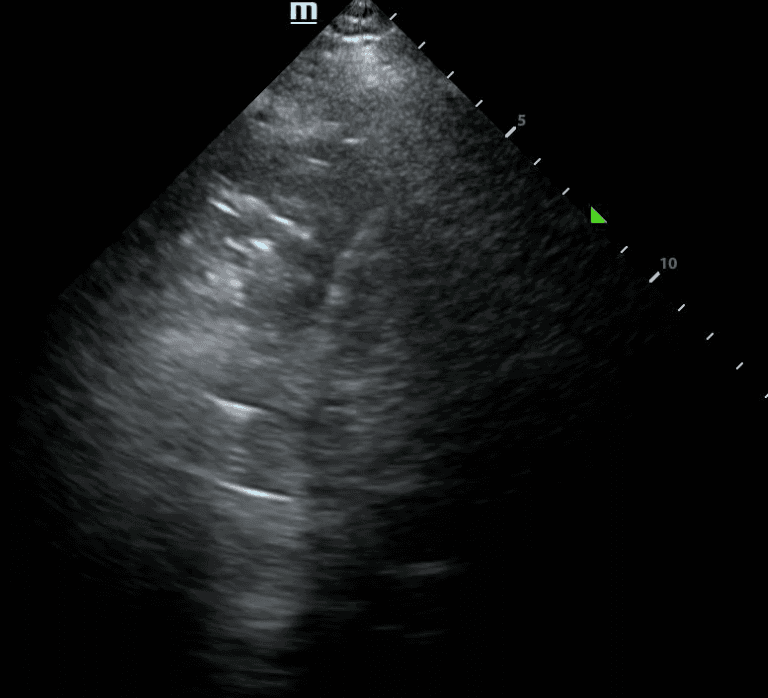
Since lung ultrasound only visualizes certain portions of the lung, we might miss some data, such as dynamic air bronchograms or increased blood flow. Patient factors such as obesity and a thick chest wall, along with the presence of dressings and chest tubes, also increase the likelihood of missing certain features. Some patients may have both atelectasis and lung consolidation, which can add uncertainty to the diagnosis. Thus, it is important to integrate ultrasound findings with the clinical picture of the patient's condition.
In sick patients, lung ultrasound surpasses chest x-rays and clinical scoring systems in diagnosing ventilator-associated pneumonia and assessing consolidations. Evidence shows that distinguishing between dynamic and static air bronchograms and evaluating for high blood flow aids in confidently discerning pneumonia from atelectasis. While valuable, these ultrasound signs aren't definitive. We integrate ultrasound findings with the broader clinical picture to develop a comprehensive assessment.
References
Winkler, M. H., Touw, H. R., van de Ven, P. M., Twisk, P., & Tuinman, P. R. (2018). Diagnostic Accuracy of Chest Radiograph, and Concomitantly Studied Lung Ultrasound, in Critically Ill Patients With Respiratory Symptoms: A Systematic Review and Meta-Analysis. Critical Care Medicine, 46(7). https://journals.lww.com/ccmjournal/abstract/2018/07000/diagnostic_accuracy_of_chest_radiograph,_and_when.45.aspx
Li, G., Cook, D.J., Thabane, L. et al. (2016). Risk factors for mortality in patients admitted to intensive care units with pneumonia. Respiratory Research, 17(80). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4940754/#:~:text=In%20this%20study%20using%20data,admitted%20to%20ICU%20with%20pneumonia.
Lichtenstein, D.; Mezière, G., Seitz, J. (2009). The dynamic air bronchogram: A lung ultrasound sign of alveolar consolidation ruling out atelectasis. Chest, 135, 1421–1425. https://journal.chestnet.org/article/S0012-3692(09)60342-1/abstract
Mongodi, S., Via, G., Girard, M. et al. (2016). B. Lung ultrasound for early diagnosis of ventilator-associated pneumonia. Chest, 149, 969–980. https://journal.chestnet.org/article/S0012-3692(15)00340-2/abstract
Mongodi, S., De Vita, N., Salve, G., et al. (2022). The Role of Lung Ultrasound Monitoring in Early Detection of Ventilator-Associated Pneumonia in COVID-19 Patients: A Retrospective Observational Study. Journal of Clinical Medicine, 11, 3001. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9181291/
Gaber, S., Tayeh, O., Wahab K. A., et al. (2021). Early detection of ventilator-associated pneumonia: Bedside tools. The Egyptian Journal of Critical Care Medicine, 7(3). https://journals.lww.com/ejccm/fulltext/2020/12000/early_detection_of_ventilator_associated.7.aspx#:~:text=Bedside%20lung%20ultrasound%2C%20CPIS%2C%20chest,prior%20to%20ventilation%20were%20excluded.
Haaksma, M. E., Smit, J. M., & Heldeweg, M. L. A. (2022). Extended lung ultrasound to differentiate between pneumonia and atelectasis in critically ill patients: a diagnostic accuracy study. Critical Care Medicine, 50(5). https://journals.lww.com/ccmjournal/abstract/2022/05000/extended_lung_ultrasound_to_differentiate_between.4.aspx
Samanta, S., Patnaik, R. Azim, A., et al. (2021). Incorporating lung ultrasound in clinical pulmonary infection score as an added tool for diagnosing ventilator-associated pneumonia: A prospective observational study from a tertiary care center. Indian Journal of Critical Care Medicine, 25(3). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7991773/
Via G, Lichtenstein D, Mojoli F, et al. (2010). Whole lung lavage: a unique model for ultrasound assessment of lung aeration changes. Intensive Care Medicine, 36(6), 999–1007. https://link.springer.com/article/10.1007/s00134-010-1834-4
SHARE
© 2025, DEEP BREATHE, INC